Is Root Canal Treatment Effective for Dental Abscess?
Dental abscesses are a serious oral health issue caused by bacterial infections in the tooth pulp or surrounding tissues. They often result in severe pain, swelling, and sensitivity, impacting daily life and overall health. Untreated abscesses can lead to complications such as bone infection or systemic spread of bacteria. Root canal treatment (RCT) is commonly recommended as a way to eliminate the infection while preserving the tooth. Understanding how effective RCT is for treating dental abscesses helps patients make informed decisions. This article explores the procedure, effectiveness, advantages, limitations, and alternative treatments.
Understanding Dental Abscesses
What is a Dental Abscess?
A dental abscess is a localized accumulation of pus caused by bacterial infection in the tooth or surrounding structures. It typically develops when bacteria penetrate the tooth pulp through cavities, cracks, or trauma. The infection triggers an immune response, leading to swelling and pain. Symptoms include throbbing toothache, sensitivity to hot or cold, fever, and facial swelling. If ignored, the infection can spread to the jawbone, sinuses, or bloodstream, causing systemic issues. Understanding the nature of dental abscesses is the first step toward effective treatment.
Types of Dental Abscesses
Dental abscesses can be categorized into three main types. A periapical abscess occurs at the tip of the tooth root, often caused by untreated cavities. A periodontal abscess develops in the gums due to gum disease, affecting the structures supporting the teeth. A gingival abscess is confined to the gums and usually results from foreign objects or localized trauma. Each type requires specific treatment, and RCT is most effective for periapical abscesses. Identifying the type accurately ensures proper management and higher chances of successful outcomes.
Causes of Dental Abscesses
Dental abscesses develop primarily due to bacterial invasion of the tooth pulp or surrounding tissues. Common causes include untreated cavities, cracked or damaged teeth, poor oral hygiene, and failed dental restorations. Systemic factors such as diabetes, immune compromise, or certain medications can also increase susceptibility. Trauma to the teeth, like fractures or repeated stress, may create pathways for bacterial entry. Early recognition of these causes allows timely intervention. Preventing abscess formation relies heavily on regular dental care and prompt treatment of oral health issues.
Root Canal Treatment: An Overview
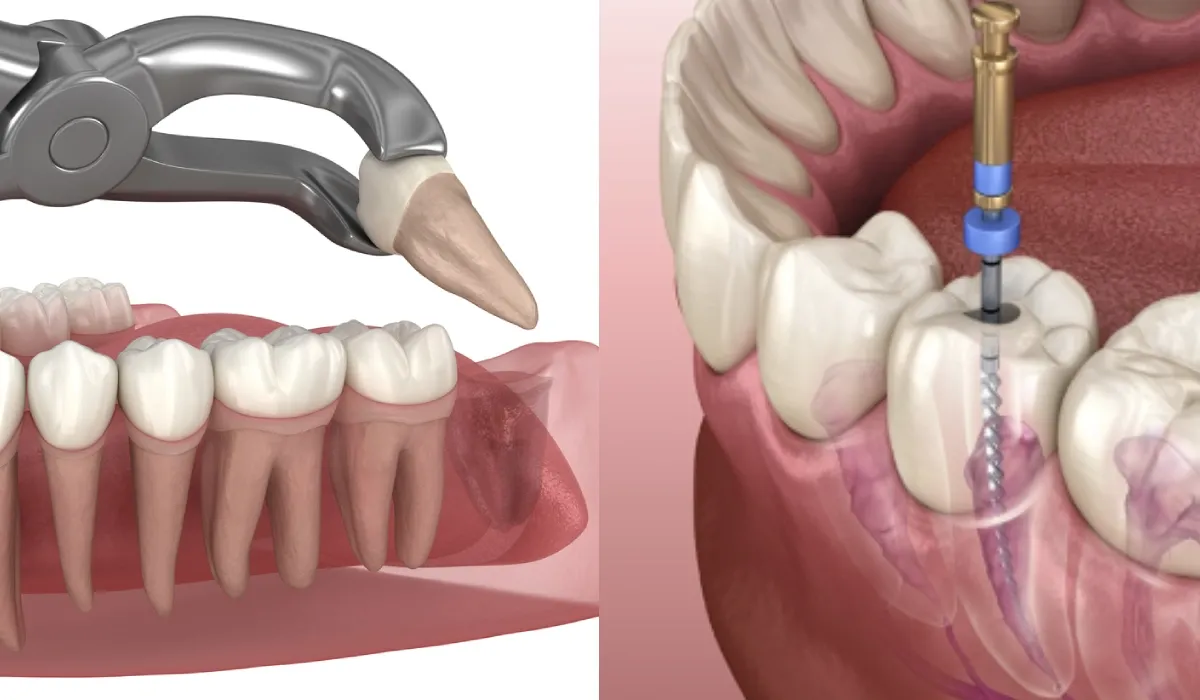
What is Root Canal Treatment?
Root canal treatment is a dental procedure designed to remove infected or damaged pulp from inside the tooth. The pulp, containing nerves and blood vessels, becomes a source of infection when exposed to bacteria. RCT cleans, disinfects, and seals the tooth canals to prevent further infection. It is a conservative treatment that allows patients to retain their natural teeth. Unlike extraction, RCT preserves the structure, function, and aesthetics of the tooth. This makes it an essential procedure for managing abscesses effectively.
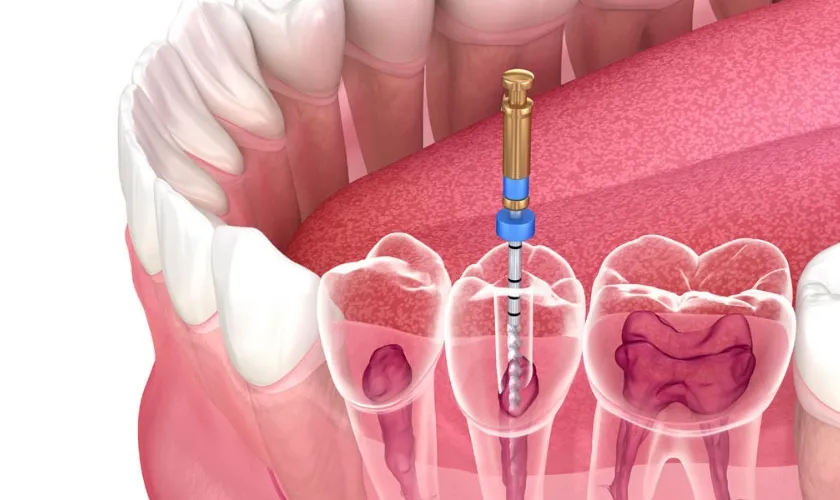
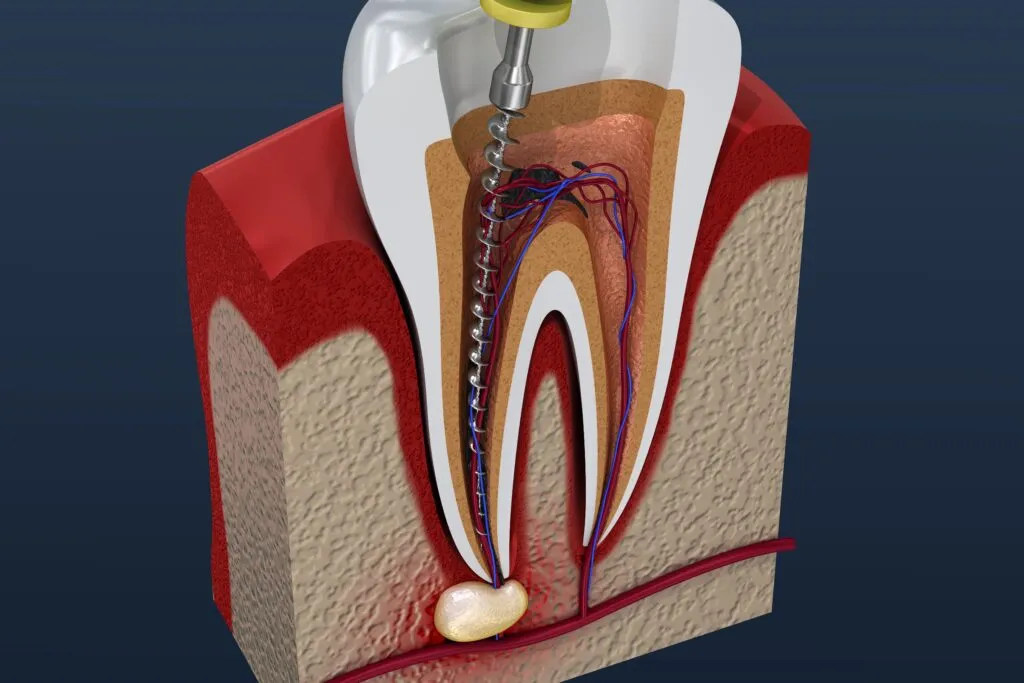
Steps Involved in Root Canal Treatment
The RCT process involves several critical steps to ensure complete removal of infection. First, a thorough diagnosis and imaging is conducted using X-rays to evaluate the infection’s extent. Then, an access opening is made to reach the pulp chamber. Cleaning and shaping remove infected tissue while preparing canals for filling. Next, disinfection eliminates remaining bacteria using antibacterial solutions. Finally, filling and sealing with gutta-percha prevent reinfection, followed by restoration with a crown or filling to restore tooth function. Each step is crucial for long-term success.
How Root Canal Treatment Addresses Dental Abscess
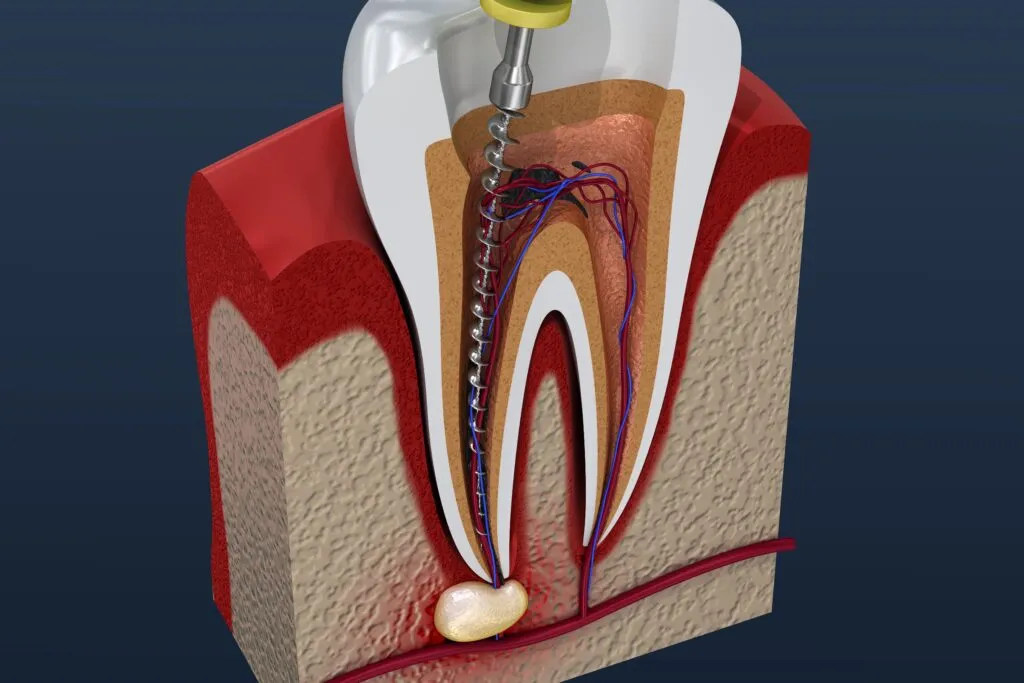
Eliminating Infection
Root canal treatment targets the root cause of dental abscesses by removing infected pulp tissue. This prevents the bacteria from spreading to surrounding bone or soft tissues. Disinfection of the canals ensures that residual bacteria are eliminated, significantly reducing the risk of recurrence. Sealing the canals with biocompatible material prevents future bacterial invasion. By removing the source of infection, RCT not only treats the abscess but also promotes the healing of surrounding tissues. It addresses both immediate symptoms and long-term oral health concerns.
Reducing Pain and Swelling
One of the immediate benefits of RCT is the reduction of pain and swelling associated with dental abscesses. The procedure removes the infected tissue, alleviating pressure and inflammation. Most patients experience significant relief within 24-48 hours, although complete healing may take several weeks. Painkillers and antibiotics may be prescribed to manage residual discomfort. The reduction in swelling also prevents the spread of infection to adjacent areas. Effective pain management is a critical measure of RCT success.
Preserving Natural Teeth
Unlike extraction, RCT allows patients to retain their natural teeth, maintaining normal chewing function and alignment. Preservation of the tooth prevents issues such as bone resorption and shifting of adjacent teeth. It also avoids the need for prosthetic replacements like implants or bridges. Retaining natural teeth contributes to better oral health, aesthetics, and self-confidence. By saving the tooth, RCT provides a long-term solution while maintaining the integrity of the dental arch.
Supporting Long-Term Oral Health
Root canal treatment contributes significantly to overall oral health by preventing the spread of infection. Untreated abscesses can cause bone loss, gum disease, or systemic complications such as heart or kidney infections. RCT removes the bacterial source and seals the canals, promoting healing. Patients can maintain proper oral function and aesthetics. Long-term follow-up ensures the treated tooth remains infection-free. This preventive aspect underscores the importance of timely root canal therapy for dental abscesses.
Effectiveness of Root Canal Treatment
Success Rate
Root canal treatment is highly effective, with success rates reported between 85% and 95%. Success is measured by resolution of infection, absence of pain, and long-term survival of the treated tooth. Proper technique and follow-up care are essential to achieve these outcomes. Even in complex cases, modern endodontic methods enhance success. High success rates make RCT a reliable treatment for dental abscesses. Patients can expect lasting relief and tooth preservation when treated appropriately.
Factors Influencing Success
Several factors affect the success of RCT. The extent of infection and bone involvement play a significant role. Tooth type matters as molars with multiple canals are more challenging to treat. Patient health, including conditions like diabetes or immune compromise, can impact healing. The skill and technique of the dentist are critical for proper cleaning, shaping, and sealing. Early intervention and adherence to post-treatment care also determine the outcome. Understanding these factors helps patients set realistic expectations.
Long-Term Outcomes
With proper restoration and oral hygiene, teeth treated with RCT can last a lifetime. Follow-ups ensure that reinfection is detected early. Retreatment or surgical intervention like apicoectomy may be needed in rare cases of persistent infection. The long-term prognosis is generally excellent when patients follow professional advice. Preserved teeth maintain chewing function, aesthetics, and jawbone integrity. This makes RCT a durable and effective solution for dental abscesses.
Advantages of Root Canal Treatment
Minimally Invasive Compared to Extraction
Root canal therapy allows patients to retain their natural teeth, avoiding the trauma of extraction. Preserving the tooth maintains normal chewing function and alignment. It also reduces the need for costly prosthetics. The minimally invasive approach promotes faster recovery and less discomfort. Patients benefit from maintaining both function and aesthetics. This makes RCT the preferred option for treating abscesses when feasible.
Effective Pain Relief
Root canal treatment directly addresses the source of infection, providing immediate relief from severe toothache. By removing infected tissue, it alleviates inflammation and swelling. Most patients report noticeable improvement within 24-48 hours. Pain management medications may be prescribed temporarily. Effective pain relief enhances patient comfort and satisfaction. It is a primary reason RCT is recommended for abscess management.
Cost-Effective in the Long Run
Although the initial cost of RCT may seem higher than extraction, it is cost-effective over time. Preserving natural teeth avoids future expenses for implants or bridges. Long-lasting restoration reduces the need for repeated dental interventions. It also prevents complications like bone loss or shifting of adjacent teeth. Considering longevity and functionality, RCT provides excellent value. It is an investment in both oral health and financial savings.
Preserves Jawbone Integrity
Retaining natural teeth through RCT prevents bone resorption that often occurs after extraction. Maintaining jawbone density supports facial structure and oral function. Extraction may require bone grafting or implants later. By preserving the tooth, RCT prevents these additional procedures. This ensures long-term oral and facial health. Patients benefit from both structural and functional preservation.
Limitations and Considerations
Not Always a Permanent Solution
While highly effective, RCT does not guarantee a permanent cure in all cases. Complex root anatomy or severe infection may require retreatment. Reinfection is possible if canals are not fully cleaned or sealed. Restoration quality also affects long-term success. Patient compliance with oral hygiene is critical. Being aware of these limitations helps set realistic expectations.
Risk of Reinfection
Reinfection can occur if bacteria remain or the tooth is not properly restored. Crowns or fillings protect against new bacterial invasion. Poor oral hygiene or trauma may also trigger reinfection. Early detection and retreatment can resolve recurring issues. Awareness of this risk ensures patients monitor their oral health. Preventive care is essential for maintaining success.
Potential Complications
Some patients may experience temporary discomfort, swelling, or mild inflammation after RCT. Rarely, complications like nerve injury or persistent infection can occur. Allergic reactions to materials or anesthesia are uncommon. Proper technique minimizes risks. Monitoring recovery and timely dental follow-up are essential. Understanding potential complications reduces anxiety and ensures safe treatment.
Alternative Treatments for Dental Abscess
Tooth Extraction
Tooth extraction is considered when the tooth is severely damaged or cannot be saved with root canal treatment. It completely removes the infected tooth and eliminates the source of infection. However, extraction results in the loss of a natural tooth, affecting chewing function and aesthetics. Patients often require prosthetic replacements like bridges or dental implants to restore function. Bone resorption can occur over time if the extraction site is left untreated. While effective at resolving the abscess, extraction is a more invasive option compared to RCT.
Incision and Drainage
In cases of rapidly spreading abscesses, dentists may perform an incision and drainage procedure to release pus. This helps reduce swelling, relieve pain, and prevent systemic spread of infection. Drainage is often combined with antibiotics to manage bacterial load. It may serve as a temporary measure before performing a root canal or extraction. The procedure is minimally invasive and provides immediate relief. However, it does not address the source of infection in the pulp, making further treatment necessary.
Antibiotic Therapy
Antibiotics are commonly prescribed to manage dental abscess infections, especially if there is swelling, fever, or systemic involvement. They help control the bacterial infection and reduce inflammation temporarily. However, antibiotics alone cannot eliminate bacteria inside the pulp chamber. Without removing the infected tissue through RCT or extraction, the abscess will likely recur. Antibiotics are best used as an adjunct to definitive treatment. They provide temporary relief but are not a standalone solution for dental abscesses.
Signs That Root Canal Treatment is Needed
Severe, Persistent Toothache – Pain that lasts several days or worsens when biting or chewing indicates pulp infection.
Swelling in Gums or Face – Visible swelling may suggest that the abscess is spreading beyond the tooth root.
Sensitivity to Hot or Cold – Increased pain from temperature changes can indicate damaged or infected pulp tissue.
Tenderness When Chewing or Touching the Tooth – Discomfort while chewing points to inflammation or abscess formation.
Presence of Pus or Bad Taste in the Mouth – A sign of active infection, indicating immediate dental intervention is needed.
Recognizing these signs early allows patients to seek timely root canal treatment, reducing the risk of complications and improving the chances of saving the tooth.
Post-Root Canal Care
Immediate Care
After RCT, patients may experience mild discomfort or swelling, which can be managed with pain relievers and prescribed antibiotics. Avoiding chewing on the treated tooth until it is fully restored is important. Gentle brushing and flossing help maintain hygiene without disturbing the area. Ice packs can help reduce swelling if needed. Following the dentist’s instructions ensures smooth recovery. Immediate care is critical for preventing reinfection or complications.
Long-Term Maintenance
Proper restoration of the treated tooth with a crown or filling is essential for long-term success. Regular dental checkups help monitor healing and detect any signs of reinfection early. Maintaining oral hygiene with brushing, flossing, and antimicrobial rinses supports overall oral health. Avoid habits like chewing hard objects or nail-biting that can damage the restored tooth. Long-term maintenance ensures that the treated tooth remains functional and infection-free.
Monitoring for Recurrence
Patients should be alert for any signs of reinfection, such as renewed pain, swelling, or discoloration. Early intervention prevents complications and preserves the treated tooth. Periodic X-rays may be recommended to check for hidden infection. Prompt retreatment or additional procedures like apicoectomy may be necessary if infection recurs. Maintaining regular follow-ups ensures long-term success. Monitoring is an essential part of post-treatment care to protect oral health.
Myths and Misconceptions
Myth 1: RCT is Extremely Painful
Many people believe that root canal treatment causes severe pain, but modern anesthesia and techniques make it relatively painless. Most patients experience relief rather than discomfort. Temporary soreness after the procedure is normal and manageable. Endodontists focus on minimizing trauma to the tooth and surrounding tissues. Education about the procedure helps reduce fear and anxiety. This myth often prevents patients from seeking timely treatment.
Myth 2: Tooth Will Become Weak After RCT
While the tooth may lose some structural strength after pulp removal, proper restoration with a crown or filling ensures functionality. Reinforced teeth can withstand normal biting and chewing forces. Modern dental materials provide durable solutions. Patients can enjoy normal oral function without increased risk of fracture. The belief that RCT teeth are fragile is largely unfounded. Effective restoration is key to preserving strength and longevity.
Myth 3: Extraction is Better Than RCT
Some people assume that removing the tooth is a better solution than performing a root canal. Extraction removes the infection but sacrifices the natural tooth. RCT preserves tooth structure, aesthetics, and function while treating the infection. Maintaining natural teeth also prevents bone loss and shifting of adjacent teeth. In most cases, RCT is a more conservative and long-term effective solution. Extraction is reserved for teeth that cannot be saved.
Case Studies and Research
Clinical Evidence Supporting RCT
Research consistently shows that root canal treatment is highly effective for periapical abscesses. Long-term studies report success rates between 85% and 95%. Advanced imaging like CBCT allows precise diagnosis and treatment planning. Proper cleaning, shaping, and sealing techniques reduce reinfection risk. Teeth treated with RCT demonstrate high survival rates over 5–10 years. Clinical evidence supports RCT as the standard of care for managing dental abscesses effectively.
Real-Life Success Stories
Many patients report immediate relief from severe pain and swelling after RCT. They regain normal oral function within days and resume daily activities comfortably. Long-term follow-ups indicate preserved teeth and improved quality of life. Patients highlight the benefits of saving natural teeth compared to extraction. Success stories reinforce confidence in root canal therapy. They demonstrate that timely and well-performed RCT effectively resolves dental abscesses while preserving oral health.
Conclusion
Root canal treatment is highly effective for treating dental abscesses, especially periapical abscesses caused by pulp infection. It eliminates infection, alleviates pain, preserves natural teeth, and supports long-term oral health. While success depends on infection severity, tooth anatomy, and patient health, modern endodontic techniques provide excellent outcomes. Proper restoration, oral hygiene, and regular follow-ups ensure the longevity of the treated tooth. Early diagnosis and timely intervention are key. RCT is a reliable, conservative, and long-term solution for dental abscess management.